
7 June 2021
Archive photo: Ashraf Hendricks
South Africa’s vaccine rollout was slow to start and even the current acceleration leaves the country far behind where it should be. A large part of the problem is global competition for vaccine supply. Yet much more needs to be done to ensure that the available vaccines get into the arms of South Africans as fast as possible.
Provinces and sites are currently performing unevenly, which should not surprise us. It is not clear how the government will address this challenge, especially as the supply of available vaccines grows.
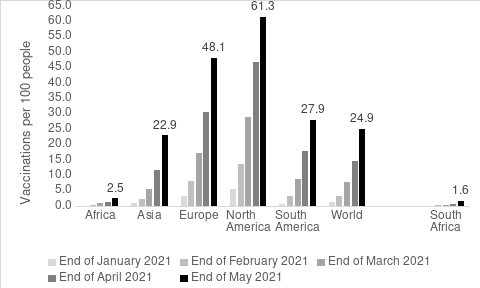
Source: Our World in Data
Africa has been at the back of the queue for vaccine delivery. By the end of May, only 2.5 vaccines had been delivered per 100 people on the continent. Yet South Africa has performed poorly even within the African context. Whereas South Africa has delivered only 1.6 vaccines per 100 people, Namibia has delivered twice this rate, and Botswana and Zimbabwe more than three times this rate. South Africa accounts for 43% of confirmed Covid-19 deaths but only 3% of vaccinations in Africa.
As of 6 June, about 500,000 people had been fully vaccinated by a single shot of the Johnson and Johnson vaccine through the Sisonke trial (for health workers) and a further almost 800,000 had received their first dose (out of a required two) of the Pfizer vaccine through the government’s vaccination programme. Yet, at that point, almost 2.5 million doses had been flown into the country. Even accounting for wastage (of 15%, because vaccinators often fail to get the full six vaccines out of each vial), delivery time and regulatory delays (related to quality control), the data suggest that South Africa had about 780,000 doses of unused vaccine in the system.
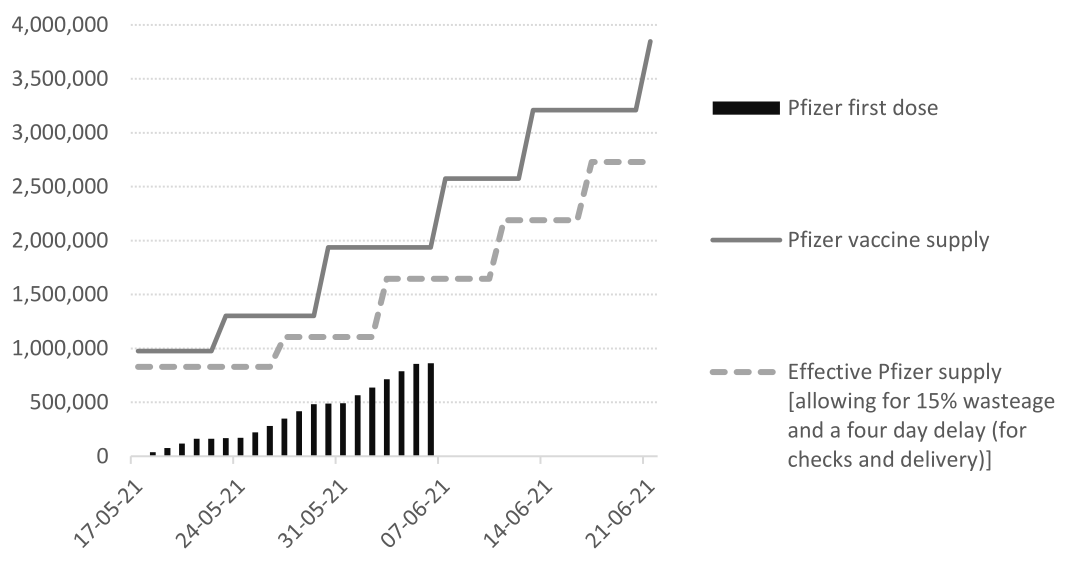
Data from government’s Coronavirus website
The government has started to release data showing how its rollout of Pfizer vaccines is progressing. This can help us see where some of this ‘surplus’ might be.
The National Department of Health currently divides the vaccine supply between private sector sites (24%) and public sector sites (76%). Private sector sites include pharmacies (especially Dis-Chem and Clicks), medical aid schemes (such as Discovery) and, at least prospectively, selected employers. The public sector supply is allocated to provinces in accordance with their share of people aged 60 or older.
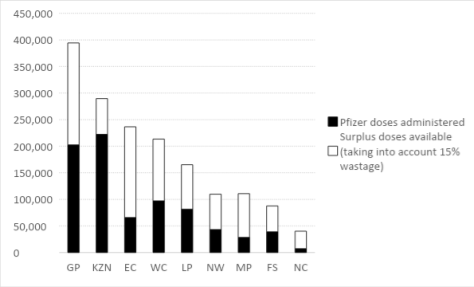
Data from government’s Coronavirus website
The above graph shows that as of midnight on 5 June, KwaZulu-Natal Province had the highest number of vaccinations. This includes vaccinations in public and private sites. We know that the public sector doses are distributed to provinces according to their share of the elderly population. We do not know how the private sector doses are distributed across provinces, but if we assume that these are also in proportion to the elderly population, then it appears that KwaZulu-Natal has been using most of its allocated supply. Most of the unused vaccine appears to be in Gauteng (22% of the national total) and the Eastern Cape (21%).
From Monday 31 May to Saturday 5 June, just over 300,000 people were vaccinated. (Very few people are being vaccinated on the weekend). At this pace, it will take about three weeks to use up the unused vaccines that are already in the country. Yet every week, an additional 636,480 doses of Pfizer arrive at OR Tambo Airport. To use up the vaccines that are already available and to use new supplies over the next two weeks, we need to more than triple our current rate of vaccination to one million doses per week.
If and when Johnson and Johnson vaccines become available, the rollout will need to accelerate even further.
The first constraint is the number of vaccination sites and hence easy access by the elderly. The number of sites was initially low but has been increasing steadily.
A second constraint was the initial requirement that elderly people await an appointment at a specified site and time. Sensibly, some sites allowed elderly people to ‘walk-in’ to those facilities rather than wait for an appointment, even registering on site rather than in advance.
A third constraint is the failure to offer vaccinations over the weekend. Extending vaccination appointments into Saturday and Sunday would substantially boost the pace of vaccinations. Additional personnel would be required, and we should start organising medical students and other qualified people (retired nurses, doctors, medical professional willing to donate their time over the weekend) to facilitate this.
A further obstacle is the delay entailed in regulatory checks and the logistical challenges with the cold chain required for the Pfizer vaccine (though we now know that it can be kept in a normal refrigerator for a month). Yet even accounting for these, there appears to be considerable quantities of unused vaccine in the system.
Some of the apparent ‘surplus’ vaccine shown in the provincial graph above may be caused by delays in reporting vaccinations, especially from sites where details of vaccinations are recorded on paper and later uploaded to the system. The National Department of Health has taken steps to encourage – or require – vaccination sites to update their stock management and vaccination systems within 24 hours. This should allow planners to identify sites where the supply of vaccines and delivery of jabs into arms is out of line.
As of midnight on 5 June, 45% of elderly South African residents had registered. The pace of registration is picking up, but very slowly. There are about two million elderly people registered on the EVDS who are waiting to be vaccinated. It is unclear how many of them will turn up for their scheduled appointments – especially those in poorer rural areas who may have to travel long distances even when all the available sites are up and running.
Given that so many people have already ‘walked-in’ to vaccination sites – and that many old age homes have already been reached – it is possible that the pace of vaccination of the elderly will slow down even as more vaccination sites are opened up.
Prioritising those over 60 for vaccination is essential. More effort is needed to register the elderly and to assist them to be vaccinated where necessary.
But this must happen in the context of an expanded rollout. The elderly should always be at the front of the queue – but we need to ensure that there are always queues, especially as the supply of available vaccines accelerates.
The original vaccination plan assumed that essential or frontline workers, and those with co-morbidities would be vaccinated as part of this phase of the rollout. Yet the EVDS system does not allow anyone younger than 60 to register.
Health workers below the age of 60 who did not register during the Sisonke trial are still being vaccinated, but their details are being verified through other platforms to ensure that only those registered with professional councils or who appear on the public sector employment data base, are vaccinated. Plans are apparently being considered to broaden vaccination among public sector workers (including teachers) as these people can also be verified through the public sector employment database. The idea of prioritising those with co-morbidities has quietly been shelved, apparently because of the administrative difficulties involved in verification.
The national and provincial health departments, and clinics and other sites on the ground, should be congratulated for accelerating the rollout over the past three weeks (albeit from a very delayed and slow start), for establishing a system that can monitor the allocation and delivery of vaccines, and for showing some flexibility and adapting the system (especially in terms of accommodating ‘walk-ins’).
Planners need to build on that flexibility to increase further the pace of vaccination. There are some obvious challenges involved.
First, will the national and provincial departments be able to divert vaccine supplies from sites (and even provinces) that are not using them expeditiously to sites (and provinces) that are, even when this is politically inconvenient?
Second, will the systems in use now be able to cope with the increased supplies of Pfizer vaccines and (we hope) J&J vaccines also? Put simply, will there be enough people at vaccination sites to ensure that vaccines are used expeditiously?
Third, will the system be able to continue to deliver vaccines to the people who need them most? There is general acceptance that the elderly need to be prioritised. But once the system is opened to younger age groups and public sector workers, it is likely to lose legitimacy, especially if those with co-morbidities are being bypassed.